Physical Address
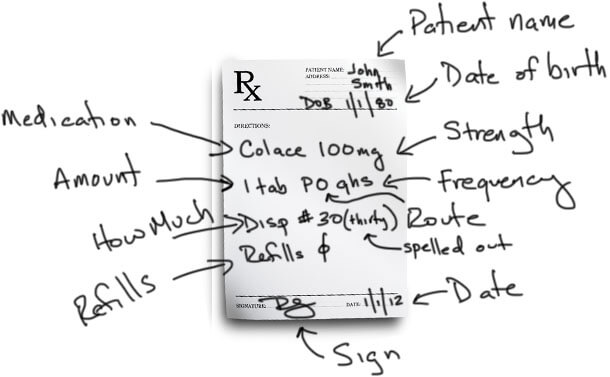
Zofran is a very popular anti-nausea medication used after surgery. You’ll notice this script is missing the “amount.” IV medications are a little different in that the amount and strength are kind of mixed together. This is not always the case, though. You also see that this is an “as needed” or “PRN” medication. When the patient complains of nausea, the nurse can give this medication because it has been prescribed.
Prescription Writing 101 (with Example Prescriptions)
I worried so much about prescription writing in my 3rd year of medical school. I probably killed a whole tree tearing up prescriptions that were wrong.
Why did I worry so much about it? Prescription writing was not covered very well at my medical school. And with the amount of material that needs to be covered in those 4 years, I wouldn’t be surprised if prescription writing isn’t covered very well at any medical school.
How to Write a Prescription in 4 Parts
- Patient’s name and another identifier, usually date of birth.
- Medication and strength, amount to be taken, route by which it is to be taken, and frequency.
- Amount to be given at the pharmacy and number of refills.
- Signature and physician identifiers like NPI or DEA numbers.
That is the basic outline of how to write a prescription. We’ll be going into the details of each step below. But first, let’s look at why it’s so important to get this skill right.
The Cost of Poor Prescription Writing
Poorly written prescriptions may be one of the main reasons there are so many medication errors today. Look at some of these commonly quoted statistics:
- Medication errors occur in approximately 1 in every 5 doses given in hospitals.
- One error occurs per patient per day.
- Approximately 1.3 million injuries and 7,000 deaths occur each year in the U.S. from medication-related errors.
- Drug-related morbidity and mortality are estimated to cost $177 billion in the U.S.
While these are just estimates from various studies and statistical models, the numbers are staggering. If there are 800,000 physicians in the United States, each physician accounts for $221,250! Do you still wonder why malpractice insurance is so expensive?
Hopefully, if you are reading this, you’re interested in not making mistakes. Even though I don’t think I caused any major harm to any of my patients with prescription errors, I wish I had read something like this when I first started writing prescriptions in my 3rd year of medical school.
How to Write Prescriptions
A prescription is an order that is written by you, the physician (or future physician), to tell the pharmacist what medication you want your patient to take. In this post, I’m going to break down all the different parts of a prescription, how to write each section, and what to look out for. Watch the video above if that’s a more appealing format to you!
Breaking Down the Prescription Format
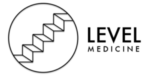
As I hinted above, here is the basic format of a prescription: First, we have the patient’s name and another patient identifier, usually the date of birth. Then we have the medication and strength, the amount to be taken, the route by which it is to be taken, and the frequency. For “as needed” medications, there is a symptom included for when it is to be taken.
The prescriber also writes how much should be given at the pharmacy and how many refills the patient can come back for. The prescription is completed with a signature and any other physician identifiers like NPI number or DEA number. Then the prescription is taken to the pharmacist who interprets what is written and prepares the medication for the patient. Now let’s look at each part of this individually.
Patient Identifiers
According to the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) national patient safety goals, at least two patient identifiers should be used in various clinical situations. While prescription writing is not specifically listed as one of these clinical situations, medication administration is. I think prescription writing should be in this category as well.
The two most common patient identifiers are their full name and date of birth. Patient identifiers are the first things to write on a prescription. This way you don’t write a signed prescription without a patient name on it that accidentally falls out of your white coat and onto the floor in the cafeteria.
Drug/Medication
This is an easy one. This is the medication you want to prescribe. It generally does not matter if you write the generic or the brand name here unless you specifically want to prescribe the brand name.
If you do want to prescribe the brand name only, you specifically need to indicate, “no generics.” There are several reasons you might want to do this, but we won’t get into that here. On the prescription pad, there is a small box which can be checked to indicate “brand name only” or “no generics.”
Strength
After you write the medication name, you need to tell the pharmacist the desired strength. Many, if not most, medications come in multiple strengths. You need to write which one you want.
Often times, the exact strength you want is not available, so the pharmacist will substitute an appropriate alternative for you. For example, if you write prednisone (a corticosteroid) 50 mg, and the pharmacy only carries 10 mg tablets, the pharmacist will dispense the 10 mg tabs and adjust the amount the patient should take by a multiple of 5.
Amount
Using my previous example for prednisone, the original prescription was for 50 mg tabs. So you would have written, “prednisone 50 mg, one tab….” (I’ll leave out the rest until we get there). The “one tab” is the amount of the specific medication and strength to take.
Again using my previous example, due to the 50 mg tabs not being available, the instructions would be rewritten by the pharmacist as “prednisone 10 mg, five tabs….” You can see that “one tab” is now “five.” Pharmacists make these changes all the time, often without any input from the physician.
Route
Up until this point, we have been using plain English for the prescriptions. The route is the first opportunity we have to start using English or Latin abbreviations. Note: It is often suggested that to help reduce the number of medication errors, prescription writing should be 100% English, with no Latin abbreviations. I will show you both and let you decide.
There are several routes by which a medication can be taken. Some common ones are by Mouth (PO), per rectum (PR), sublingually (SL), intramuscularly (IM), intravenously (IV), and subcutaneously (SQ).
As you can see, the abbreviations are either from Latin roots like PO (“per os”) or just common combination of letters from the English word. Unfortunately, when you are in a hurry and scribbling these prescriptions, many of these abbreviations can look similar. For example, intranasal is often abbreviated “IN,” which, if you write sloppily, can be mistaken for “IM” or “IV.”
Common route abbreviations for prescription writing:
- PO (by mouth)
- PR (per rectum)
- IM (intramuscular)
- IV (intravenous)
- ID (intradermal)
- IN (intranasal)
- TP (topical)
- SL (sublingual)
- BUCC (buccal)
- IP (intraperitoneal)
Frequency
The frequency is simply how often you want the patient to take the medication. This can be anywhere from once a day, once a night, twice a day, or even once every other week. Many frequencies start with the letter “q.” This Q is from the Latin word quaque, which means once.
So in the past, if you wanted a medication to be taken once daily, you would write QD, for “once daily” (“d” is from “die,” the Latin word for day). However, to help reduce medication errors, QD and QOD (every other day) are on the JCAHO “do not use” list. So you need to write out “daily” or “every other day.”
Common frequencies abbreviations for prescription writing:
- daily (no abbreviation)
- every other day (no abbreviation)
- BID/b.i.d. (twice a day)
- TID/t.id. (three times a day)
- QID/q.i.d. (four times a day)
- QHS (every bedtime)
- Q4h (every 4 hours)
- Q4-6h (every 4 to 6 hours)
- QWK (every week)
The “Why” Portion
Many prescriptions that you write will be for “as needed” medications. This is known as “PRN,” from the Latin pro re nata, meaning “as circumstances may require.” For example, you may write for ibuprofen every 4 hours “as needed.”
What physicians and medical students commonly miss with PRN medications is the “reason.” Why would it be needed? You need to add this to the prescription. You should write “PRN headache” or “PRN pain,” so the patient knows when to take it.
How Much
The “how much” instruction tells the pharmacist how many pills should be dispensed, or how many bottles, or how many inhalers. Typically, you write the number after “Disp #.”
I highly recommend that you spell out the number after the # sign, even though this is not required. For example, I would write “Disp #30 (thirty).” This prevents someone from tampering with the prescription and adding an extra 0 after 30, turning 30 into 300.
Refills
The last instruction on the prescription informs the pharmacist how many times the patient can use the same exact prescription, i.e. how many refills they can get.
For example, let’s take refills for oral contraceptives for women. A physician may prescribe 1 pack of an oral contraceptive with 11 refills, which would last the patient a full year. This is convenient for both the patient and physician for any medications that will be used long term.
Prescription Writing Examples
This example is a common medication prescribed when people are leaving the hospital. It is one 100 mg tablet, taken at bedtime. The prescription is for 30 pills and no refills.
Zofran is a very popular anti-nausea medication used after surgery. You’ll notice this script is missing the “amount.” IV medications are a little different in that the amount and strength are kind of mixed together. This is not always the case, though. You also see that this is an “as needed” or “PRN” medication. When the patient complains of nausea, the nurse can give this medication because it has been prescribed.
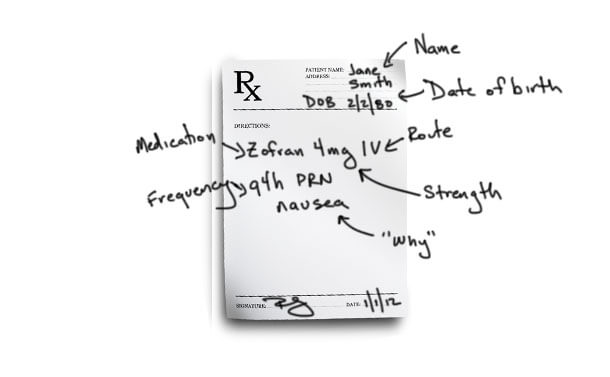
This example shows a common way to write prescriptions for liquids, especially for children. Here I’ve used the word “liquid” as a placeholder for the name of a liquid medication. Liquids come in specific strengths per amount of liquid. Here, the strength is 10 mg per 5 mL. We only want to give 5 mg, though, so the “amount” that we prescribe is only 2.5 mL per dose. It’s given by mouth every 4 hours. We are dispensing “1 (one) bottle”. You could also just write “1 (one)” as the pharmacist would know what you mean.
To finish up, here is a list of the JCAHO “Do Not Use” List:
- U or u (unit) – use “unit”
- IU (International unit) – use “International Unit”
- Q.D./QD/q.d./qd – use “daily”
- Q.O.D./QOD/q.o.d./qod – use “every other day”
- Trailing zeros (#.0 mg) – use # mg
- Lack of leading zero (.#) – use 0.# mg
- MS – use “morphine sulfate” or “magnesium sulfate”
- MS04 and MgSO4 – use “morphine sulfate” or “magnesium sulfate”
Links and Other Resources
How to Write a Prescription: 7 Steps for Safety

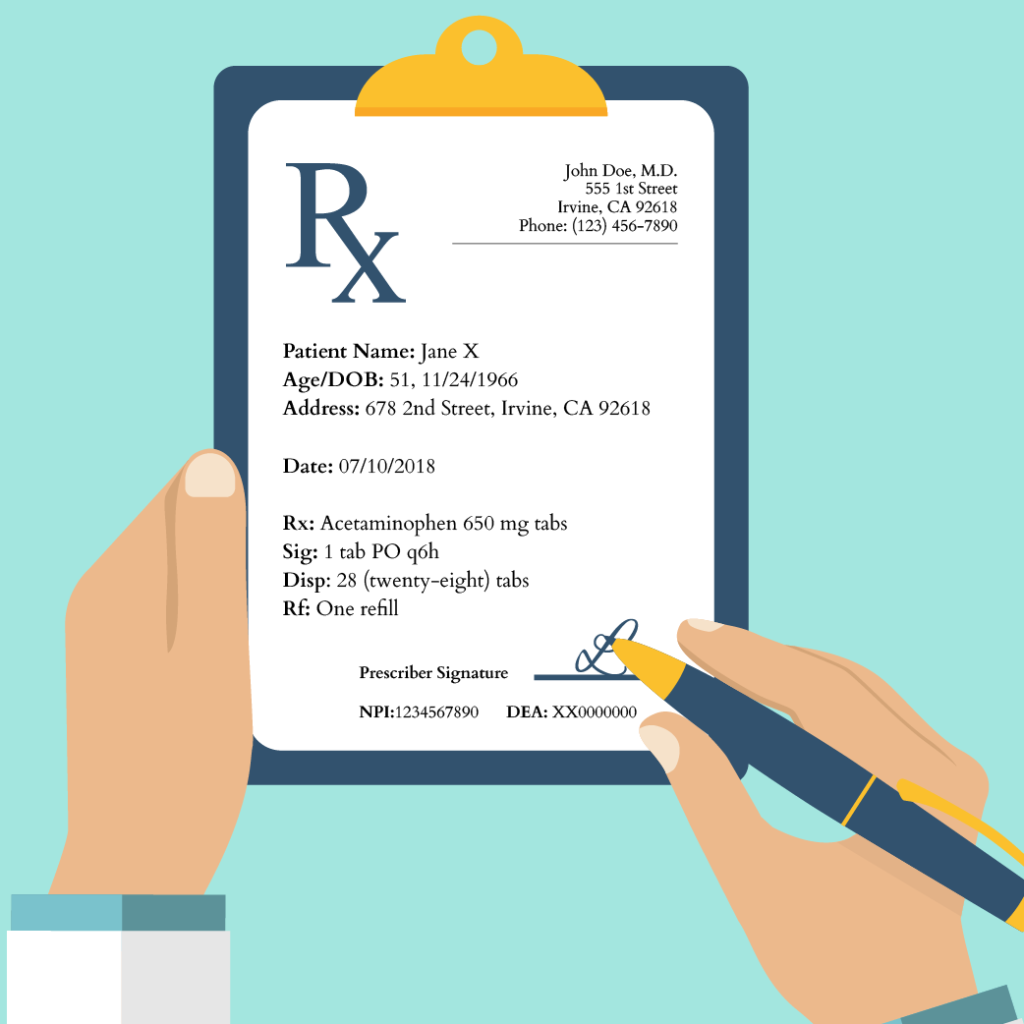
Are you learning to write a prescription? It’s not that difficult once you know the seven steps to write a prescription safely. Every drug prescription consists of seven parts: the prescriber’s information, the patient’s information, the recipe (the medication, or Rx), the signature (the patient instructions or Sig), the dispensing instructions (how much medication to be dispensed to the patient or Disp), the number of refills (or Rf), and the prescriber’s signature (including his or her National Provider Identifier and/or Drug Enforcement Agency number). Below are each of these sections in detail.
Time needed: 3 minutes
How to write a prescription in 7 steps:
- Prescriber’s Information This information is usually found at the top of the prescription. It generally consists of the prescribing clinician’s name, office address, and contact information (usually the office’s telephone number).
- Patient’s Information Below the prescriber’s information is the patient’s information. This section will include the patient’s full name, age, and date of birth. Sometimes the patient’s home address will be found here, as well. You should also specify the date you wrote the prescription.
- Recipe (Rx) The recipe should include the medication being prescribed, its dose, and its dosage form. For example, if you are prescribing 650 milligrams (mg) tablets of acetaminophen, you would write “acetaminophen 650 mg tablets” or “acetaminophen 650 mg tabs.”
- Signatura (Sig) After the recipe is the signature, the signature (Sig) gives the patient instructions on how to take the medication. The Sig should include information on how much drug to take, how to take it, and how often to take it.
For example, if you would like your patient to take one 650 mg tablet of acetaminophen every six hours, you would write “Take 1 tablet by mouth every six hours” or, using abbreviations, “1 tab PO q6h.”
So for our hypothetical acetaminophen example, our prescription looks like this:
In 2020, over four and a half billion prescriptions were filled at pharmacies across the United States. Given their sheer prevalence, prescriptions are a key source of medical errors. In fact, prescription errors account for 70% of medication errors that result in harm. Thus, it is crucial that all clinicians master the ability to properly write a prescription.
In learning to write a prescription properly, it is worth discussing two common sources of prescription errors. First, if you are handwriting your prescription, make sure that it is legible. While e-prescribing is increasingly making handwritten prescriptions a thing of the past, you will likely have to manually prescribe medications at some point in your career. Illegible prescriptions are a source of frustration for patients, pharmacists, and other medical providers, and can increase the risk of medication errors. No matter how busy you are, it is always better to spend a few extra seconds slowly writing out a legible prescription than risk your patient’s health.
Always be cautious when using abbreviations. While abbreviations are commonly used in medicine, you should keep in mind that the risk of a medication error is increased when abbreviations are ambiguous or misused. So if you choose to use abbreviations in your prescriptions, be sure only to use well-known ones (commonly used medical abbreviations can be found here). If you are unsure whether you should use an abbreviation, spend the extra few seconds to write out your directions completely.

Kunal Sindhu, MD, is an assistant professor in the Department of Radiation Oncology at the Icahn School of Medicine at Mount Sinai and New York Proton Center. Dr. Sindhu specializes in treating cancers of the head, neck, and central nervous system.