Physical Address
ERAS has decided to break up the residency locations into the following geographic sections:
The Supplemental ERAS Application: Everything You Need to Know (2022)
A guide to completing the new supplemental ERAS application

Part 1: Introduction
Part 2: The past experiences section
Part 3: The geographic information section
Part 4: The preference signaling section
Part 1: Introduction
Applying to residencies is complicated, and the pressure to get everything from your USMLE scores to your personal statement to your NRMP rank order list in shipshape order is undoubtedly stressful. Fortunately, you’ve likely known about and have been preparing for this process since beginning medical school.
In June 2021, the AAMC announced that applicants to residency programs in certain specialties would have the option of completing a supplemental application in addition to the main ERAS application. Originally limited to just internal medicine, surgery, and dermatology programs, the supplemental ERAS application will be used by programs in 16 specialties during the 2022–2023 application cycle.
If you’re applying to residencies in one of these participating specialties, the idea of a supplemental application may have induced panicky flashbacks of writing countless secondary essays during your med school application cycle.
Breathe easy—the supplemental ERAS application is far less involved. Still, you want to complete it with the same care and consideration that you’d apply to any other part of your residency applications.
In this guide, we’ll go over everything you need to know about the supplemental ERAS application. We’ll walk you through how to complete each section so you can have the greatest chances of matching into your top-choice residency program.
What is the supplemental ERAS application?
The supplemental ERAS application is a relatively short, three-section application that asks questions about your most meaningful experiences, geographic preferences, and preferred residency programs. The AAMC estimates that it should take most applicants fewer than 60 minutes to complete, though we recommend carving out at least a few hours to think through your responses.
According to the AAMC, the supplemental application was created so residency programs could learn more about applicants’ interests and experiences, allowing programs to recognize candidates who best fit their mission, goals, and environment. The AAMC notes that programs may use the supplemental application data in a variety of ways, including as part of the initial application screening, as a secondary screening, or as a companion to the residency interview process.
You might groan at the thought of adding another step to the residency application process, but there are a couple pieces of good news: first, the supplemental application is free to complete. Second, you only need to fill it out once—the same responses will be sent to all participating programs to which you’re applying.
Who should complete the supplemental ERAS application? Which specialties are participating in the supplemental ERAS application?
The supplemental ERAS application is currently being used by residencies in the following specialties:
- Adult Neurology
- Anesthesiology
- Dermatology
- Diagnostic Radiology and Interventional Radiology
- Emergency Medicine
- General Surgery
- Internal Medicine (Categorical)
- Internal Medicine/Psychiatry
- Neurological Surgery
- Obstetrics and Gynecology
- Orthopedic Surgery
- Pediatrics
- Physical Medicine and Rehabilitation
- Preventive Medicine
- Psychiatry
However, not every program in those specialties is electing to use the supplemental application, and some specialties have only opted into using certain sections of the application. Therefore, you’ll want to check the individual requirements for each program and specialty to which you plan to apply. The AAMC provides lists of participating residency programs in each of these specialties (note: the 2022–2023 list will be available in July 2022).
All applicants who register for myERAS will receive an invitation via email to complete the supplemental application, regardless of which specialty they plan to apply in. Furthermore, all questions and sections in the supplemental ERAS application are optional, as is the application itself. So, should you complete it?
If you are applying to programs in one of the above participating specialties, we recommend that you do. The opportunity to provide more information about yourself may help you stand out to the programs in which you’re most interested, and given that the application is relatively brief, it doesn’t require a major investment of time. Plus, since the supplemental application is still relatively new, we don’t yet know how programs will view applicants who elect to leave it blank.
When should you complete the supplemental ERAS application?
The supplemental ERAS application can be completed any time between August 1st and September 16th.
In the pilot year, supplemental applications were transmitted to residency programs in two groups, depending on the date applications were submitted. However, it now appears that all supplemental applications will be transmitted to programs on September 28th, regardless of the date of submission.
Take note that you must register for an ERAS token by September 14th at the very latest in order to receive an invitation to complete the supplemental application in time.
What questions are on the supplemental ERAS application?
The supplemental ERAS application is divided into three sections: the past experiences section, the geographic information section, and the preference signaling section. Below, we’ll provide an overview of each section, as well as guidance and strategic thinking on how to answer each question.
Part 2: The past experiences section
The past experiences section asks you to identify up to five experiences that were particularly meaningful or impactful during your path towards residency. Although you’ll already have listed plenty of experiences on your ERAS application’s activities section and your medical student CV, programs want to learn which experiences have been most influential in shaping your career goals and development as a future physician.
Note that programs in emergency medicine and obstetrics and gynecology will not receive answers from this section.
You can list experiences that occurred during medical school or beforehand, and you can include anything from clinical work to volunteering to extracurricular activities. Below are the types of experiences that you can choose from when classifying your experiences:
- Education/training
- Military service
- Professional organizations
- Research
- Teaching/mentoring
- Volunteer/service/advocacy
- Work
- Other extracurricular activities, clubs, or hobbies
For each experience, you’ll enter basic information detailing what the experience was and how involved you were—expect to provide data like your position title, the organization’s name, the start and end dates of your involvement, and so on. Clinical, research, and volunteer experiences will also trigger additional fields specific to those types of experiences.
You can find a full list of the information you’ll need to provide in the AAMC’s valuable Supplemental ERAS Application Guide.
For each experience, you’ll also be asked to write 300 characters describing why the experience was meaningful, what you learned, and how it influenced your career development and goals. 300 characters is short—just two or three sentences—so you must be succinct.
Here’s an example:
Volunteering in the community garden program gave me insight into the lack of access to fresh produce faced by many Angelenos. It was rewarding to help people in my neighborhood obtain healthy foods, and it reinforced my belief that good nutrition is an important aspect of preventative care.
Other impactful experiences section
The past experiences section also includes a 750-character space to describe other impactful experiences. Here, you’ll have the opportunity to provide information about your background or life experiences that haven’t come up elsewhere in your application, such as in your personal statement.
It’s important to note, however, that this question is specifically interested in obstacles you’ve overcome, and it’s not expected that all applicants will respond to it. If you haven’t faced a significant obstacle on your way towards or through medical school, you’ll probably want to skip this question.
Here’s a list of examples provided by the AAMC of the types of experiences you might describe here:
- Your family background (e.g., you’re a first-generation college student)
- Your financial background (e.g., your family is low income or you had to work to support your family growing up)
- The setting of the community you grew up in (e.g., a lack of access to healthcare or a high crime rate)
- Your educational experiences (e.g., you had limited educational opportunities)
- Other life circumstances (e.g., you lost a family member or you had to serve as a caregiver while working or in school)
This list of examples isn’t exhaustive, but it should give you a sense of the types of experiences that merit a response.
Let’s take a look at an example answer:
I grew up working in my family’s convenience store after school. As a result, I didn’t participate in extracurriculars and did most of my studying behind the store counter. When it came time to apply to college, I had little guidance—neither of my parents had attended college—so I applied to my state’s flagship public university but was rejected. Following graduation, I enrolled in community college, where I became passionate about biology. After earning my associate’s, I transferred to Ohio State, the same school that had rejected me two years earlier. While my path has been less straightforward than many of my peers, I’m grateful to understand the barriers that far too many face and which I want to work to lessen as a physician.
Part 3: The geographic information section
In this section, you can let residency programs know more about the locations that interest you most. This can be especially useful if you’re hoping to attend residency in a part of the country in which you have no obvious ties, a situation that might otherwise cause a program to pass you over out of doubt that you’d actually relocate.
For example, say you’ve lived your whole life in California but your significant other just took a job in Boston. Choosing New England on your supplemental application will allow you to demonstrate that you’re serious about the possibility of moving.
You’ll be given the opportunity to choose up to three out of nine geographic regions in which you’d most prefer to attend residency. You can also indicate that you have no preference or that you do not want to communicate a preference. Again, note that your responses in this section won’t be shared with programs in emergency medicine and obstetrics and gynecology.
Here are the regions you’ll choose from:
- Pacific West: AK, CA, HI, OR, WA
- Mountain West: AZ, CO, ID, MT, NM, NV, UT, WY
- West North Central: IA, KS, MN, MO, NE, ND, SD
- East North Central: IL, IN, MI, OH, WI
- West South Central: AR, LA, OK, TX
- East South Central: AL, KY, MS, TN
- South Atlantic: DC, DE, FL, GA, MD, NC, SC, VA, WV
- Middle Atlantic: NJ, NY, PA
- New England: CT, ME, MA, NH, RI, VT
For each region that you select (or if you select that you have no preference), you’ll be given 300 characters in which to explain your choice.
I was born in Philadelphia and lived there until my family relocated to Colorado when I was twelve. I’m eager to move back to the Mid-Atlantic region to be closer to my extended family, who still reside in and around Philadelphia.
Note that a regional preference, along with its accompanying essay, will only be shared with programs in that region. However, if you indicate no preference or leave the question blank, this information will be shared with all programs.
You’ll also be asked to rate your degree of preference for urban vs. rural settings, and you’ll again have 300 characters to elucidate why.
I grew up in a small town in New Hampshire and attended college in Maine. While I’ve enjoyed the amenities of city life during medical school in Chicago, I hope to eventually return to a slower-paced, quieter environment with greater access to nature.
Part 4: The preference signaling section
The preference signaling section is where you’ll express your interest in specific residency programs. Although you’ll likely apply to numerous programs, here you can send a signal of especial interest to a select group of the programs that appeal to you most. Depending on which specialties you’re applying in, you’ll be able to send different numbers of signals—for example, you can signal up to 3 programs in dermatology, up to 7 in internal medicine, and up to 30 in orthopedic surgery.
Similar to the geographic information section, the intention of this section is to help program directors identify the most interested candidates, rather than waste interview invites on candidates with whom they are unlikely to match. Sending a program a signal of interest may especially help less competitive candidates differentiate themselves from stronger applicants who are applying to the program as a backup.
Filling out this section is straightforward: simply select the names of the programs you want to signal from the drop-down menu. However, do note the following:
- If you’re applying in certain specialties such as dermatology, emergency medicine, and internal medicine, you shouldn’t signal a residency program at your medical school or a program where you completed an in-person away rotation or sub-internship. These programs will assume you have a strong interest in matching with them regardless. If you’re applying in other specialties, you are free to signal programs with which you already have an affiliation.
- Your choices aren’t ranked, so the order you select them in doesn’t matter.
- Programs will only be able to see whether or not you’ve signaled their program. They won’t know who else you’ve signaled or whether you’ve signaled any programs at all.
Preference signaling strategies
Of the three sections, the preference signaling section is the one that may require the most strategic thinking. Should you signal interest in “reach” programs in order to boost your chances, or should you choose less competitive programs so you can maximize your chances of matching somewhere? Moreover, how can you really know which programs interest you most before you’ve even interviewed?
While there’s always the chance that you’ll change your mind about a program after interviewing, spend some time assessing which programs are the best fit for you in terms of how their missions and environments mesh with your own goals and interests.
Furthermore, consider the strength of your application relative to a program’s competitiveness. Signaling programs that are reaches for you might pay off, but you might also waste opportunities to make an impression on programs you can more easily match with. Conversely, it’s smart to send signals to less competitive “safety” programs to increase your overall odds of matching, but you don’t want to inadvertently prevent yourself from matching with your dream program, either.
Therefore, we suggest signaling a range of programs. Aim for a mixture of 1–2 reaches, 2–3 targets, and 1–2 safeties, and adjust these numbers accordingly depending on the number of signals available.
Final thoughts
Since the supplemental application is still in an early phase, we don’t fully know how it will impact programs’ choices of whom to interview or the likelihood that a candidate will match. However, data from the pilot year demonstrates that programs placed varying degrees of emphasis on different parts of the application. In addition, when it came to the geographic and preference signaling sections, the vast majority of programs used the information gathered as part of their holistic review processes, often in order to break ties and identify worthy candidates who had been previously overlooked.
According to the AAMC, the questions that wind up being most useful to programs may eventually be integrated into the main ERAS application, and the supplemental application will subsequently be discontinued. Until then, by allowing you to provide residency programs with more information about yourself, the supplemental ERAS application can help you stand out to the programs that most interest you and with which your goals and experiences best align.
A Guide to ERAS Supplemental Applications for 2023 Match Cycle
medschoolcoach ![]()
![]()
![]()
![]()

Table of Contents
- What is the Supplemental ERAS Application?
- What are the sections of the Supplemental ERAS Application?
- Which specialties require the Supplemental ERAS Application?
- What is the deadline for the Supplemental ERAS Application?
- The Past Experiences Section
- Geographic Preference Section
- What is Preference/Program Signaling (PS)?
- How do I decide where to assign my signals?
- Should I signal my home institution in the Supplemental ERAS Application?
- Should I signal away rotations?
What is The Supplemental ERAS Application?
Starting in 2021, the The Electronic Residency Application Service® (ERAS®) began offering a supplemental application designed to help students share more about themselves. This was also designed to assist program directors in finding applicants that fit their programs’ setting and mission. This is especially important given that in January 2022, USMLE Step 1 went Pass/Fail, which put a new spin on residency applications. Previously, program directors were able to rely on Step 1 as a screening mechanism, but without it, they were left with one less tool to use. The ERAS Supplemental Application is an adjunct tool for program directors to choose applicants.
What Happens When USMLE Step 1 Goes Pass Fail?
What are the sections of the Supplemental ERAS Application?
The supplemental ERAS application is broken into three sections. We’ll cover all three sections here in this guide with links below.
Which specialties require the Supplemental ERAS Application?
It started with just two, but has slowly become more and more. We anticipate there maybe even more in 2024. The following specialties will participate in the ERAS supplemental application process for the 2022-23 application cycle. The table below breaks down the specialties, along with which parts of the Supplemental ERAS application they participate in. Keep in mind,
| ERAS Specialty | Supplemental Experiences | Geographic Preferences | Preference Program Signals (# of programs you can signal) |
| Adult Neurology | Yes | Yes | 3 |
| Anesthesiology | Yes | Yes | 5 |
| Dermatology | Yes | Yes | 3 |
| Diagnostic Radiology and Interventional Radiology | Yes | Yes | 6 |
| Emergency Medicine | No | No | 5 |
| General Surgery | Yes | Yes | 5 |
| Internal Medicine (Categorical) | Yes | Yes | 7 |
| Internal Medicine/Psychiatry | Yes | Yes | 2 |
| Neurological Surgery | Yes | Yes | 8 |
| Obstetrics and Gynecology | No | No | 3 |
| Orthopedic Surgery | Yes | Yes | 30 |
| Pediatrics | Yes | Yes | 5 |
| Physical Medicine and Rehabilitation | Yes | Yes | 4 |
| Preventive Medicine | Yes | Yes | 3 |
| Psychiatry | Yes | Yes | 5 |
What is the deadline for the Supplemental ERAS Application?
For the 2023 cycle, the deadline to submit was Friday September 16th 2022. While this deadline was present, keep in mind that the actual ERAS can’t be reviewed by residency programs until September 28th. The rationale for the Supplemental Application to be due earlier is unclear, but those are the rules that ERAS put in place!
The Past Experiences Section
Drawing upon a similar trend with the most meaningful experiences section of the AMCAS application, the ERAS now has a past experiences section where you can showcase up to 5 of your most 5 most important and meaningful experiences. There is also an additional essay where you can share another impactful experience that demonstrates a challenge or a hardship you faced on your journey to medicine.
The character limits of the past experiences section is only 300 characters, so you do not have a lot of space here!
You need to fill in the following information for each of the 5 meaningful experiences:
The Position title
The Organization name
Your Start and end dates
The Frequency of participation (This is always tricky, because some experiences may be daily for just a period of time. Just use your best judgement)
Setting (rural vs urban). Rural is defined as population of ≤2500 while urban is defined as population of ≥50,000
Experience type: explains what type of experience you had. The following categories are included:
- Education/training (includes clinical training such as clerkships, away rotations, sub-internships, structured observerships, etc.)
- Military service
- Professional organization (includes societies, associations, etc., at the local, regional, national, or international levels)
- Other extracurricular activity, club, hobby (includes sports, music, theater, student government, etc.)
- Research
- Teaching/mentoring (includes paid teaching positions such as high school teacher as well as teaching assistant, tutor)
- Volunteer/service/advocacy (includes unpaid experiences, service, advocacy)
- Work (includes paid clinical, nonclinical
Primary focus area. The following categories are included:
- Basic science
- Clinical/translational science
- Community involvement/outreach
- Customer service
- Health care administration
- Improving access to health care
- Medical education
- Music/athletics/art
- Promoting wellness
- Public health
- Quality improvement
- Social justice/advocacy
- Technology
Key characteristic: This should demonstrate the most important characteristic you got out of this experience. The following characteristics are included:
- Communication
- Critical Thinking and Problem Solving
- Cultural Humility and Awareness
- Empathy and Compassion
- Ethical Responsibility
- Ingenuity and Innovation
- Reliability and Dependability
- Resilience and Adaptability
- Self-Reflection and Improvement
- Teamwork and Leadership
You are only allowed to pick one experience type, one primary focus area, and one key characteristic for each of the 5 experiences.
Description of the experience (maximum 300 characters including spaces): Explain why this experience is meaningful and how it influenced you. Do NOT describe what you did in the experience as this is already mentioned in your CV.
The other impactful experiences section asks the following question:
“Please describe any challenges or hardships that influenced your journey to residency. This could include experiences related to family background, financial background, community setting, educational experiences, and/or general life experiences.”
Here, applicants have the opportunity to share any challenges they faced throughout their medical journey. Programs do not expect all applicants to complete this question as not everyone faced such a challenge or hardship. But if you faced one, it is highly recommended that you include it here. There is a character limit of 750 characters including spaces. We recommend not going overboard here. If you don’t have a truly impactful statement to write, it’s best to skip out here.

Geographic Preference Section
ERAS has decided to break up the residency locations into the following geographic sections:
- Pacific West: AK, CA, HI, OR, WA
- Mountain West: AZ, CO, ID, MT, NM, NV, UT, WY
- West North Central: IA, KS, MN, MO, NE, ND, SD
- East North Central: IL, IN, MI, OH, WI
- West South Central: AR, LA, OK, TX
- East South Central: AL, KY, MS, TN
- South Atlantic: DC, DE, FL, GA, MD, NC, SC, VA, WV
- Middle Atlantic: NJ, NY, PA
- New England: CT, ME, MA, NH, RI, VT
As a residency applicant, you get to choose up to three of these nine sections. Then, with just 300 characters, you can explain each of your preferences. For example, you might illuminate ties you have to the region, such as family or ancestry in the location. Your geographic preference will only be shared with programs in that geographic area.
Rural vs. Urban Signaling
Unlike the geographical signaling that only programs within a region would see, all programs can view the urban/rural descriptions.
What should you include in the past experiences section of the supplemental ERAS?
It’s totally up to you as the applicant what you’d like to include here, but you probably want to consider including research experience in the speciality you are applying into. This is important because program directors will often look to applicants research as a way to gauge interest in a speciality, as well as future potential in the field.
What is Preference/Program Signaling (PS)?
PS allows an applicant to send a limited number of “signals” to residency programs that they are genuinely interested in at the time of the initial residency application. These signals help programs identify genuinely interested applicants early in the application review process, providing an opportunity for a more holistic review of applicants most interested in their program.
There is a real history to program signaling. In fact, there are even academic papers that are written about it. An editorial in the Western Journal of Emergency Medicine Dec 2021 written by Alexis Pelletier-Bui et al states:
Preference signaling is a concept rooted in game theory and developed in labor economics to address the challenge of employers not being able to perform a detailed analysis of all potential applicants and aiding them with identifying high-yield employee prospects. Preference signaling allows applicants to assign virtual “tokens” to their most desired employers, providing applicants the opportunity to communicate their interest, and employers the ability to focus their attention on these most “serious” applicants.
How do I decide where to assign my signals?
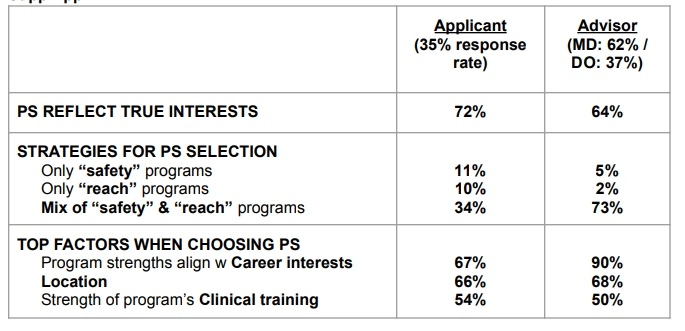
PS is new to the residency application process, therefore there is a paucity of data available on how to best assign signals. Most advice provided in this document is based on consensus and not in evidence. The data we do have is from other specialties and best practices may differ by specialty. We do have some information on how advisors advised applicants to use their signals, and how applicants decided to utilize their signals via the ERAS SuppApp in the 2021-2022 residency application cycle, reflected in the table below, referenced from the CodeEM Applicant/Advisor Supplemental Guide
How Advisors Advised and Applicants Utilized Signals in the 2021-2022 ERAS
Because signals will be assigned in concert with ERAS submission, it is strongly recommended that applicants spend some time researching programs and reflecting on what their priorities are in a prospective training program as they are putting together their initial application. There will be more opportunity to learn and reflect in depth on programs during the interview and ranking phase of the process, but having an understanding of some basic program information and the characteristics of applicants that have been accepted in the past can go a long way to helping applicants select the programs they plan to signal. There will not be a post-interview round of signals.
Let’s consider some examples. It is likely to be low yield to use a signal if your USMLE/COMLEX scores are well below a program’s cut off for consideration or if you only have a COMLEX score and a program does not consider COMLEX scores in lieu of USMLE. If you are an IMG and a program denotes US grads only, does not sponsor visas, or has no track record of matching IMGs, using a signal with that program is likely to be low yield. Make sure to consider statistics and probabilities, realizing that the yield of your signal will be lower in these situations compared to utilizing your signals at programs with applicant/resident characteristics that may match more closely with your own
Conversely, it is not wise to use a signal on a program where you are already likely to be offered an interview, such as a home institution (although the AAMC has slightly differing advice on this, see below).
Should I signal my home institution in the Supplemental ERAS Application?
This is a question that is asked a lot. In general, signaling home institutions should not be needed because they should know you as the applicant. This is especially true if you know the program well. Most program directors will tell you this, but you should check individually with your PD to see if they want you to signal (hint, if you meet with them in person, that’s basically signaling that you are interested in their residency program).
Should I signal away rotations?
Similar to a home institution, you probably already have a great chance of getting an interview at a place you participated in an away rotation for. For this reason, we don’t necessarily recommend signaling those programs. Instead, it maybe best to save your signal for programs where you aren’t quite as well know. That said, the AAMC has published a table where they suggest signaling home and away institutions, however our suggestion at MedSchoolCoach is to show your face with the program director instead and express your interest in person, rather than just via the ERAS.
| Specialty | Signal home | Signal away rotation programs |
| Adult Neurology | Yes | Yes |
| Anesthesiology | Yes | Yes |
| Dermatology | No | No |
| Diagnostic Radiology and Interventional Radiology | Yes, unless the home program tells you not to. | Yes |
| Emergency Medicine | No | No |
| General Surgery | Yes | Yes |
| Internal Medicine (Categorical) | No | No |
| Internal Medicine/Psychiatry | Yes | Yes |
| Neurological Surgery | Yes | Yes |
| Obstetrics and Gynecology | Yes | Yes |
| Orthopedic Surgery | Yes | Yes |
| Pediatrics | Yes, unless the home program tells you not to. | Yes |
| Physical Medicine and Rehabilitation | Yes | Yes |
| Psychiatry | Yes, unless the home program tells you not to. | Yes |
| Public Health and General Preventive Medicine | Yes | Yes |


Read Full Bio
Sahil Mehta MD
Founder, MedSchoolCoach
Dr. Mehta is a Harvard trained interventional radiologist and one of the foremost experts on medical school admissions in the country. He is a nationally known expert in prostate artery embolization. He has personally overseen and guided hundreds of applicants into and through medical school, as well as developed tools and training for MedSchoolCoach advisors to help thousands of students a year.