Physical Address
Testosterone : a steroid hormone produced primarily in the male testes and responsible for the development of male secondary sex characteristics
Male Reproductive System Mcat
The gonads are the precursors of the genitalia in males that mostly include external (penis, scrotum, epididymis, and testes) and in females that mainly include internal (vagina, uterus, fallopian tubes, cervix, and ovary) organs; genitalia allow males and females to mate, fertilize internally, and support the growth and development of offspring.
Testosterone causes undeveloped tissues to differentiate into male sexual organs. When testosterone is absent, the tissues develop into female sexual tissues. Primitive gonads become the genitalia , testes or ovaries. Tissues that produce a penis in males produce a clitoris in females. The tissue that will become the scrotum in a male becomes the labia in a female; that is, they are homologous structures.
Most of the male reproductive system is located outside of the body (external structures) and includes penis, scrotum, epididymis, and testes. The internal organs or the accessory organs include the vas deferens, seminal vesicles, prostate gland, and bulbourethral glands.
- Penis : The male organ for sexual intercourse and urination. It delivers urine.
- Scrotum: A loose, pouch-like sack of skin that hangs behind the penis, containing the testes. It carries and supports testes.
- Epididymis: Located at the back of the testis and connects it to the vas deferens. This is where the sperm fully matures and becomes motile, and it functions to store and carry sperm.
- Testis: The location for testosterone production. The coiled collection of tubes within the testes are the seminiferous tubules. Within these tubules, spermatogenesis takes place.
- Vas deferens : Transports mature sperm to the urethra in preparation for ejaculation.
- Seminal vesicles : Sac-like pouches that attach to the vas deferens near the base of the bladder. It contributes to semen production.
- Prostate gland : A walnut-sized structure located below the urinary bladder in front of the rectum. It also contributes to semen production.
- Bulbourethral (Cowper’s) glands : Pea-sized structures located on the sides of the urethra just below the prostate gland. These glands produce a clear, slippery fluid that cleans urethra at ejaculation.
The functions of the male reproductive system include producing and transporting sperm, ejaculating sperm into the female reproductive tract, and producing and secreting male hormones.
The organs of the male reproductive system are specialized for three primary functions:
- To produce, maintain, transport, and nourish sperm (the male reproductive cells) and protective fluid (semen).
- To discharge sperm within the female reproductive tract.
- To produce and secrete male sex hormones.

Consequently, several reproductive structures are exterior to the female’s body. These include the breasts and the vulva, which consists of the mons pubis, clitoris, labia majora, labia minora, and the vestibular glands. Internal female reproductive structures include ovaries, oviducts, the uterus, and the vagina.
- Mons pubis : A round, fatty area that overlies the pubic symphysis.
- Clitoris : A structure with erectile tissue that contains a large number of sensory nerves and serves as a source of stimulation during intercourse.
- Labia majora : A pair of elongated folds of tissue that run posterior from the mons pubis and enclose the other components of the vulva. It covers the labia minora
- Labia minora : Thin folds of tissue centrally located within the labia majora and covers vestibule.
- Greater vestibular glands : Found at the sides of the vaginal opening and provide lubrication during intercourse.
- Breast : Consists of mammary glands and fat. It produces and delivers milk.
- Ovaries: Held in place in the abdominal cavity. They carry and develop eggs.
- Oviductsor Fallopian tubes : Extend from the uterus in the lower abdominal cavity to the ovaries, but they are not in contact with the ovaries. They transport eggs to the uterus.
- Uterus : A structure about the size of a woman’s fist. It supports the developing embryo and fetus during gestation. The cervix is the lowermost portion of the uterus.
- Vagina : A muscular tube that serves as a common tube for intercourse, birth canal, and passing menstrual flow.
The human female reproductive system (or female genital system) contains two main parts and functions differently:
- Hosts the developing fetus
- Produces vaginal and uterine secretions
- Passes the anatomically male sperm through to the fallopian tubes
- Produce the anatomically female egg cells.
- Produce and secrete estrogen and progesterone

Practice Questions
Khan Academy
MCAT Official Prep (AAMC)
Online Flashcards Biology Question 1
Biology Question Pack, Vol. 1 Passage 18 Question 104
Practice Exam 2 B/B Section Question 57
Key Points
• Primitive gonads become the genitalia, testes or ovaries; tissues that produce a penis in males produce a clitoris in females while the scrotum in a male becomes the labia in a female; that is, they are homologous structures.
• The functions of the male reproductive system include producing and transporting sperm, ejaculating sperm into the female reproductive tract, and producing and secreting male hormones.
• The female reproductive system contains two main parts: the uterus, which hosts the developing fetus, produces vaginal and uterine secretions, and passes the anatomically male sperm through to the fallopian tubes; and the ovaries, which produce the anatomically female egg cells.
• Most of the male reproductive system is located outside of the body that includes the penis, scrotum, epididymis, and testes; internal organs or the accessory organs include the vas deferens, seminal vesicles, prostate gland, and bulbourethral glands.
• A female’s internal reproductive organs are the vagina, uterus, fallopian tubes, cervix, and ovary; external structures include the mons pubis, pudendal cleft, labia majora and minora, vulva, Bartholin’s gland, and the clitoris.
Key Terms
Semen contains spermatozoa, proteolytic and other enzymes, and fructose that promotes spermatozoa survival. It also provides a medium for sperm motility
Testosterone : a steroid hormone produced primarily in the male testes and responsible for the development of male secondary sex characteristics
Vulva : consists of the female external genital organs
Primitive Gonads: formed by the proliferation of germ cells
Genitalia: a sex organ
Reproduction and Development for the MCAT: Everything You Need to Know
Learn key MCAT concepts about reproduction and development, plus practice questions and answers
(Note: This guide is part of our MCAT Biology series.)
Table of Contents
Part 1: Introduction to reproduction and development
Part 2: Reproductive overview
a) Endocrine control
b) Spermatogenesis
c) Oogenesis
Part 3: Fertilization and early development
a) Fertilization
b) Cleavage, blastulation, and implantation
c) Gastrulation
Part 4: Germ cell layers
a) Endoderm
b) Mesoderm
c) Ectoderm
Part 5: Neurulation
Part 6: Later development
a) Stages of pregnancy
b) Cell specialization
c) Apoptosis and regeneration
Part 7: High-yield terms
Part 8: Passage-based questions and answers
Part 9: Standalone questions and answers
Part 1: Introduction to reproduction and development
As you review the anatomy, physiology, and biochemistry of the human body, it may seem almost miraculous that the human body can reproduce in such a short amount of time. In as little as eight weeks after fertilization, a single-celled zygote quickly becomes a multicellular embryo with many developing organ systems.
In this guide, we will briefly review the endocrinology and cellular physiology of reproduction. Then we’ll dive into the key stages of development: from fertilization leading to blastulation, then gastrulation and neurulation. Finally, at the end of this guide, you’ll be able to apply what you’ve learned using practice problems and an MCAT-style practice passage.
Let’s get started!
Part 2: Reproductive overview
a) Endocrine control
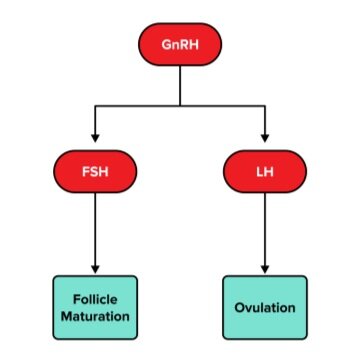
The hypothalamus, anterior pituitary, and gonads make up the hypothalamic-pituitary-gonadal axis, or HPG axis. The hypothalamus releases a hormone called gonadotropin-releasing hormone (GnRH), which acts on the anterior pituitary gland. In response, the anterior pituitary gland secretes follicle-stimulating hormone (FSH) and luteinizing hormone (LH). You can find more information on the hypothalamus and pituitary glands in our guide on the endocrine system.
FSH and LH are both hormones that act directly on the gonads and have different effects on male and female bodies. In females, FSH acts on the ovaries to stimulate the growth and maturation of follicles: immature cells that assist in the development of eggs. In males, FSH will stimulate spermatogenesis, or the production of sperm.
In females, LH triggers ovulation and promotes estrogen production. Estrogen thickens the endometrium, which is the lining of the uterus. It also encourages the development of secondary sexual characteristics in females. Additionally, LH also promotes progesterone synthesis during the menstrual cycle. Together, these hormones determine the onset of folliculogenesis, ovulation, and the luteal phase.
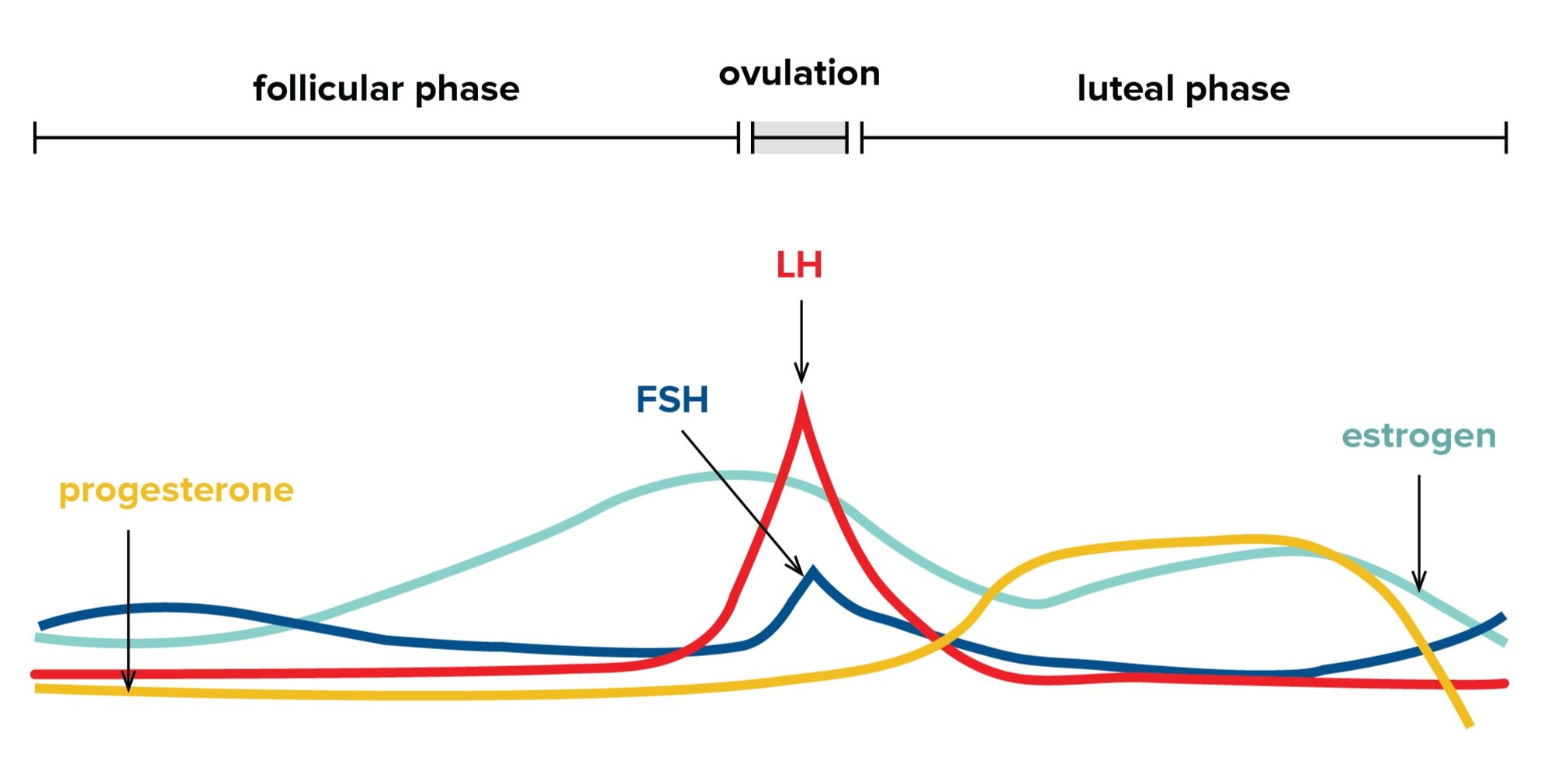
In males, LH stimulates testosterone synthesis. During puberty, this hormone promotes the development of secondary sexual characteristics in males and stimulates sexual drive. However, this hormone is also crucial for a male fetus as it promotes the development of male genitalia.
In early development, early embryos are “sexually indifferent”: while their chromosomal sex is already determined, their genitalia and sex cells are not yet induced to become male or female. The presence of testosterone is crucial in inducing the early genitalia to follow a male course of development.

In normal physiology, male and female germ cells develop into different structures. Recall that the testes are male structures that store sperm, or male germ cells. The ovaries are female structures that store eggs, or female germ cells. These two sets of germ cells require specialized sets of helper cells to assist in their development: the development of sperm requires Sertoli cells and Leydig cells, while the development of oocytes requires granulosa cells and theca cells. The production of sperm and egg cells is collectively referred to as gametogenesis, as they result in the production of gametes.
b) Spermatogenesis
The male reproductive anatomy consists of both internal and external structures. The testes are the male gonads.
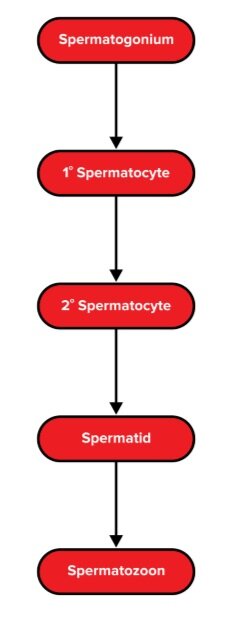
Spermatogenesis is the process through which sperm are formed in the seminiferous tubules of the testes. First, a diploid spermatogonium undergoes mitosis to form a diploid primary spermatocyte. After undergoing meiosis I, two haploid secondary spermatocytes are formed. Both of these then undergo meiosis II to form four haploid spermatids. The spermatids undergo further maturation and finally develop into spermatozoa.
This meiotic division and maturation occur in long, coiled structures within the testes called seminiferous tubules. Spermatogenesis is aided by Sertoli cells (specialized cells in the seminiferous tubules of the testes and are stimulated by FSH) and Leydig cells (cells that are also found in the testes and are stimulated by LH to produce testosterone).
Sperm acquire motility and await ejaculation in a structure called the vas deferens. After maturation, each of these spermatids becomes a haploid spermatozoon. When ejaculation occurs, sperm will pass through the vas deferens, the ejaculatory duct, and then the urethra, which facilitates its exit from the penis.